Many times, I receive panic calls from patients expressing a desperate need to meet me urgently due to concerns about their health. When I consult them, I often find that the individual is completely asymptomatic and has come in primarily for a routine checkup, during which it is revealed that their cholesterol or triglyceride levels are elevated. This raises a significant question: is high cholesterol truly a death sentence? Can a patient with a deranged lipid profile unexpectedly face life-threatening events? In this blog post, I will endeavor to clarify these concerns in brief by explaining the fundamentals of cholesterol metabolism, its various health effects on the body, and the effective treatment options available for managing hypercholesterolemia. Understanding these aspects is crucial for individuals to become more aware of their health and the implications of lipid levels in their overall well-being.
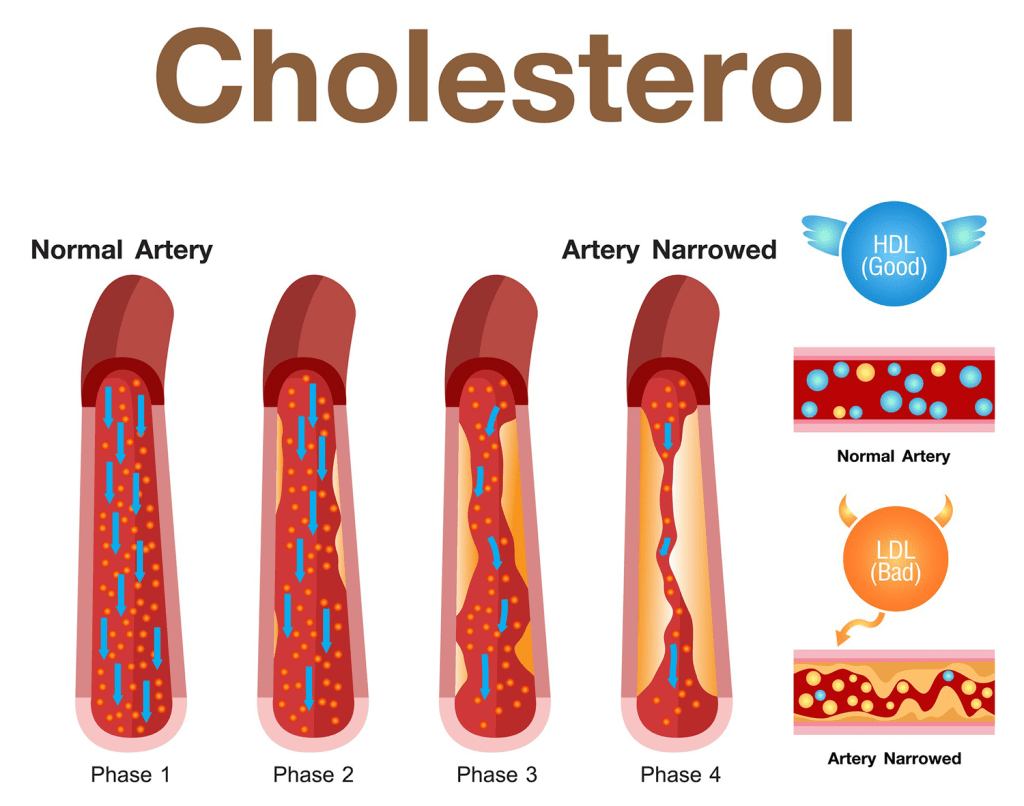
Cholesterol is a basic building block of our body, playing a crucial role in various physiological processes. The main mechanism of these organic chemicals is to carry various types of lipids from one part of the body to another, ensuring that cells receive the necessary fats for energy and structural integrity. There are various types of cholesterol molecules, and the detailed biochemistry is quite complex; hence we will discuss two main molecules first: high-density lipoprotein cholesterol (HDLC) and low-density lipoprotein cholesterol (LDLC). HDLC is often called “good cholesterol” because this molecule takes excess cholesterol from the bloodstream to the liver, where it is metabolized or excreted, thereby preventing the formation of lipid plaques and subsequently avoiding blockages in the arteries. On the other hand, LDLC is referred to as “bad cholesterol” as it carries cholesterol from the liver to the blood vessels, increasing the risk of plaque formation, which can later grow into significant blockages, potentially leading to heart disease or stroke. Therefore, maintaining low levels of LDLC while ensuring high levels of HDLC is essential for good health and cardiovascular well-being. Apart from these, one more molecule is crucial: triglycerides (TG). High levels of triglycerides are detrimental to heart health and can adversely affect other blood vessels as well. Specifically, dyslipidemia is a term that refers to high levels of LDLC and triglycerides, along with low levels of HDLC, and addressing this imbalance is vital for reducing the risk of cardiovascular diseases and promoting overall wellness. Regular check-ups and lifestyle modifications, including a balanced diet and exercise, can help manage cholesterol levels effectively.
Two factors are most importantly associated with dyslipidemia: one is an unhealthy diet, and the other is a lack of exercise. A diet rich in food items that can increase LDLC and triglycerides (TG) often includes an excess of saturated fatty acids, which can be found in products such as coconut oil, ghee, butter, and cream. These ingredients, while flavorful and popular in many cuisines, can significantly contribute to dyslipidemia when consumed frequently and in large quantities. On the other hand, oils that contain a good amount of polyunsaturated fatty acids, such as sunflower oil and olive oil, are generally considered healthier alternatives. However, it is important to note that moderation is key; even these healthier oils can be detrimental when taken in excess. Furthermore, non-vegetarian food items, particularly those that contain red meat and animal fats, also pose risks, as they are typically high in saturated fatty acids, which can further exacerbate health issues associated with dyslipidemia. Besides unhealthy lipids, an excessive intake of carbohydrates has also been implicated in the development of dyslipidemia, especially through the elevation of triglycerides. Simple carbohydrates, such as sugar or sugary products and even jaggery, can lead to lipid dysregulation if consumed in large amounts, contributing to an imbalance in lipid profiles. In contrast, complex carbohydrates—when consumed in moderate amounts—are beneficial for health and can be found in wholesome foods such as fruits and vegetables, which provide essential nutrients and fiber. Mind you, anything in excess, no matter how healthy, can lead to adverse effects, so it is crucial to maintain a balanced diet and an active lifestyle to promote overall health and well-being.
Lack of exercise is a very important reason for dyslipidemia. Our previous generations used to take a good amount of saturated fats like ghee; however, they were actively engaged in exertional work such as farming and other physically demanding tasks, which undoubtedly contributed to their metabolic health and prevented the onset of dyslipidemia. In stark contrast, present-day lifestyles often involve long hours of sitting and minimal physical activity, leading to a sedentary life coupled with high-calorie and high-fat diets that are rich in processed foods and sugars. This combination significantly increases the risk of developing various health problems, including dyslipidemia, obesity, and cardiovascular diseases. Therefore, incorporating daily aerobic exercises, such as brisk walking, jogging, cycling, and swimming, for at least 30 to 40 minutes is crucial for maintaining a healthy lipid profile. In addition to these aerobic activities, incorporating stretching exercises such as yoga helps improve flexibility and reduce stress levels, while engaging in muscle strengthening exercises, like moderate weight training at the gym, enhances overall body composition and metabolic rates. A holistic approach that combines these elements not only promotes better cardiovascular health but also contributes to improved overall well-being, ensuring that individuals can lead healthier, more active lives.
In the modern era, the excessive amounts of stress, coupled with a lack of sleep, lead to elevated levels of adrenaline and corticosteroids in the body, which are primarily responsible for the increase in low-density lipoprotein cholesterol (LDLC) and triglyceride (TG) levels. Furthermore, these new risk factors contribute to a decrease in high-density lipoprotein cholesterol (HDLC) levels, further exacerbating the situation and significantly increasing the risk of atherosclerosis. The interplay between stress, sleep deprivation, and lipid levels underscores the importance of a balanced lifestyle and effective stress management techniques to maintain optimal health and reduce the risk of these serious complications.
Another important cause of dyslipidemia is genetic tendency. There are multiple forms of hypercholesterolemia and hypertriglyceridemia, where the patient has a tendency to develop high levels of low-density lipoprotein cholesterol (LDLC) or triglycerides (TG), or both simultaneously. This genetic predisposition can manifest in various forms, often leading to significant health issues if not managed properly. These elevated lipid levels can result in blockages in blood vessels at an early age, contributing to one of the leading causes of sudden cardiac deaths in young people, a tragic outcome that underscores the importance of early detection and intervention. Furthermore, the Indian population exhibits a concerning tendency to have elevated LDLC and TG, making individuals in this demographic particularly vulnerable to developing coronary arterial disease and cerebrovascular diseases, conditions that can severely impact quality of life and increase mortality risk. Hence, understanding the genetic factors contributing to dyslipidemia is critical for developing targeted screening and prevention strategies tailored to at-risk populations.
Diagnosis of dyslipidemia is a straightforward process that primarily hinges on performing a proper fasting lipid profile. For accurate results, a fasting period of 12 to 14 hours is necessary. A common mistake made by both patients and general practitioners is relying solely on total cholesterol levels, which offer limited insight into a patient’s lipid health. Another significant error is conducting this test in a non-fasting state, as the results, particularly for triglyceride (TG) levels, can fluctuate considerably. Reliable interpretation of lipid levels is essential for effective treatment planning and management.
Every individual should undergo this lipid profile test upon reaching 40 years of age to assess their cardiovascular risk accurately. Those diagnosed with hypertension (HTN), type 2 diabetes mellitus (T2DM), heart disease, or a history of stroke are advised to have this test performed every six months. In some cases, testing may need to occur even more frequently, especially if adjustments to medication dosages are necessary based on lipid levels. Furthermore, younger patients with a family history of coronary artery disease or stroke should also get tested earlier in life to allow for early detection and intervention.
Over a period of the last 3 to 4 decades, a variety of drugs have become available for the effective treatment of high cholesterol and triglyceride levels. Statins have emerged as the cornerstone of treatment for high low-density lipoprotein cholesterol (LDL-C) levels, primarily due to their ability to reduce the risk of cardiovascular events by effectively lowering LDL-C. They function by inhibiting the HMG-CoA reductase enzyme, which plays a crucial role in the production of cholesterol in the liver.
In addition to statins, medications such as fenofibrate and niacin are also available for patients who experience very high triglyceride (TG) levels that remain uncontrolled by statins alone. These medications offer alternative pathways for lipid management, with fenofibrate focusing on lowering TG levels and enhancing HDL cholesterol levels, while niacin functions to both lower LDL and TG levels and increase HDL levels.
As research and clinical practices have advanced, new classes of medications have emerged. Drugs like ezetimibe, which works by inhibiting the absorption of cholesterol in the intestines, and bempedoic acid, a more recent addition that blocks cholesterol synthesis, have broadened the therapeutic arsenal for managing dyslipidemia. Moreover, in the last decade, the introduction of injectable therapies has revolutionized treatment strategies, particularly for patients who may not achieve their LDL-C targets with oral medications alone.
The latest innovation in this field is inclisiran, a novel therapeutic agent that operates similarly to a vaccine in its mechanism of action. This drug facilitates a decrease in LDL-C levels and is administered via an injection once every six months, offering a significant convenience for long-term management of cholesterol.
Furthermore, the treatment goals for different clinical subsets of patients can widely vary. For instance, in young, healthy individuals, the target for LDL-C levels is typically set below 100 mg/dL to maintain optimal cardiovascular health. Conversely, for patients diagnosed with coronary artery disease who exhibit multiple blockages, healthcare providers may adopt a more aggressive stance on treatment, lowering the target LDL-C level to 30 mg/dL or lower. This stratification of treatment goals emphasizes the importance of individualized care and highlights the necessity of tailoring lipid-lowering strategies to meet the specific needs of each patient.
Regular doctors consultation is advisable for initiating and titrating the doses of the medications, as these visits provide essential guidance and monitoring for patients. Doctors decide the dosages of the medications depending on the risks and tolerance of the patient, ensuring a tailored approach that maximizes safety and efficacy. It is crucial for patients to understand that many who stop medications after noticing their cholesterol levels appear normal, according to laboratory standards, are making a common but potentially dangerous mistake. This misjudgment can lead to serious health consequences, as many high-risk individuals need to take medications lifelong, regardless of whether their cholesterol levels return to a normal range. Management of cholesterol should be seen as a long-term commitment to health and well-being, requiring continuous follow-up and adjustments based on individual progress and changes in health status. Regular consultations allow physicians to evaluate the effectiveness of the treatment plan and make necessary modifications to secure optimal health outcomes for their patients.
In conclusion high cholesterol is not a death sentence—but ignoring it can be dangerous. Dyslipidemia is a silent, progressive condition that often shows no symptoms until it causes serious events such as heart attack or stroke. The reassuring truth is that with timely detection, lifestyle modification, and appropriate medical therapy, cholesterol-related risks can be significantly reduced or even neutralized. A healthy diet, regular physical activity, stress control, and adequate sleep form the foundation of prevention, while modern lipid-lowering medications provide powerful protection for those at higher risk. Most importantly, cholesterol management is not a one-time correction but a lifelong partnership between the patient and the physician. Understanding your numbers, following medical advice consistently, and avoiding premature discontinuation of therapy can make the difference between preventable disease and long-term cardiovascular health.
Dr. Tamiruddin A. Danwade
Consultant Interventional Cardiologist.
Dr. Tamiruddin A. Danwade is a highly skilled Consultant Interventional Cardiologist known for his expertise in managing complex cardiovascular conditions. His dedication to patient care and commitment to advancing medical practices in cardiology have earned him a stellar reputation in the field.
He operates primarily out of two esteemed locations: the Mother & Rhythm Clinic, located in the vibrant neighborhoods of Seawoods and Kharghar, where he provides specialized care tailored to meet the individual needs of his patients. His hands-on approach in this clinic ensures that each patient receives comprehensive assessments and personalized treatment plans that consider their unique medical histories and lifestyle factors.
In addition to his work at the Mother & Rhythm Clinic, Dr. Danwade is also associated with BV Medicover Hospitals in Navi Mumbai. This facility is renowned for its state-of-the-art technology and a multidisciplinary approach, allowing for collaboration among various medical professionals to deliver holistic care. Dr. Danwade is an integral part of the cardiovascular team at the hospital, where he employs cutting-edge interventional techniques to treat a spectrum of heart-related issues.
With a focus on preventative care and patient education, Dr. Tamiruddin A. Danwade strives to empower individuals with the knowledge they need to maintain optimal heart health, thereby improving their quality of life. His work continues to impact many lives, making him a pivotal figure in the cardiology community.

Leave a comment